- Home
- Health Center
- Health Info
- Atopic Dermatitis & Sensitive Skin
Allergy
Atopic Dermatitis & Sensitive Skin
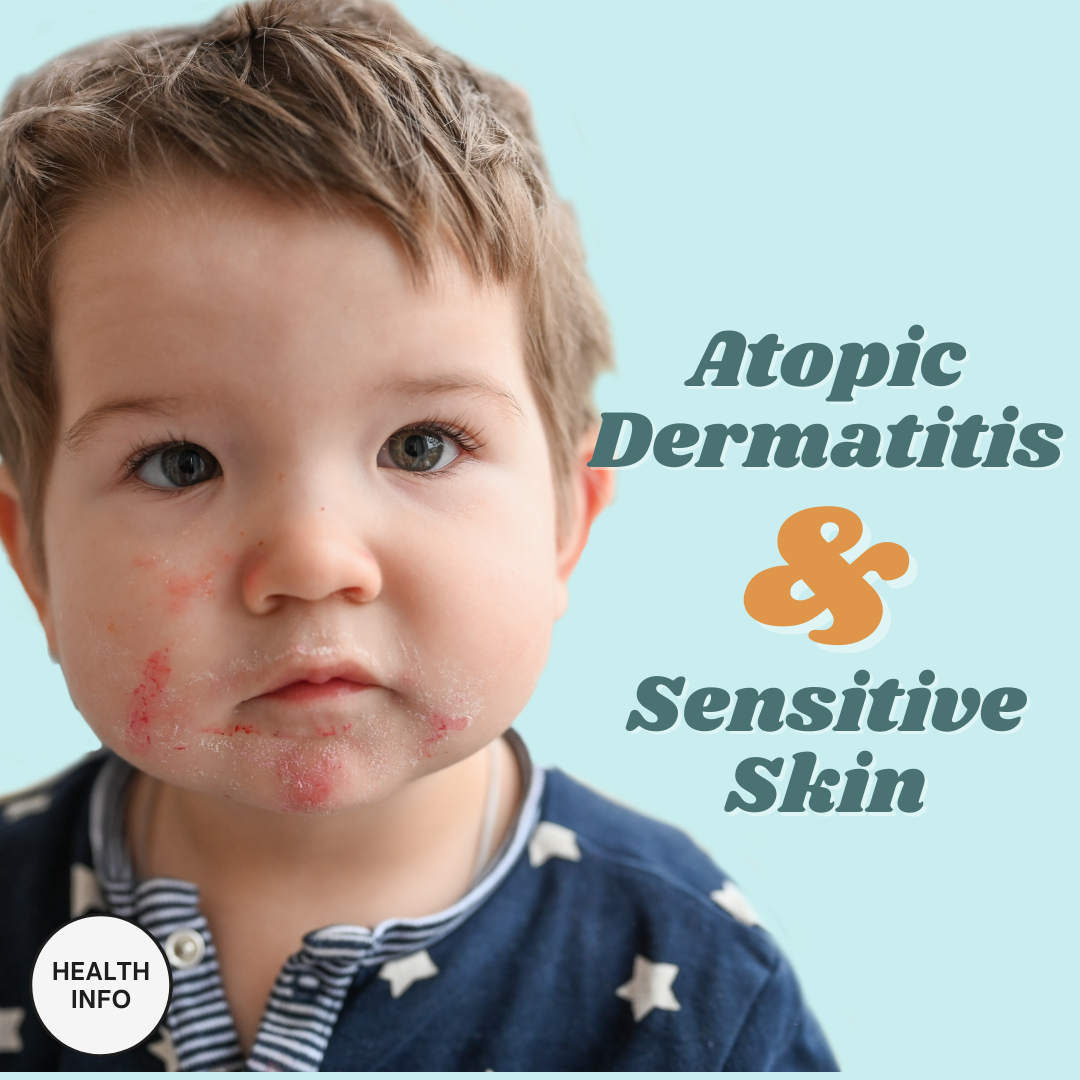

What is Atopic Dermatitis?
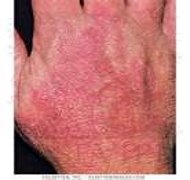
Atopic dermatitis (AD), or more known as eczema is a chronic or recurrent, non contagious skin inflammation, characterized by dry skin and itch. AD often occurs in sensitive areas such as the face, neck, flexures (see pictures below). In Malaysia, the prevalence of AD is about 20%, with 90% of patients developing the condition before the age of five.


AD Symptoms
AD signs and symptoms vary widely from person to person and include:
- Dry skin
- Itching
- Thickened, cracked, scaly skin
- Skin redness
- open, crusted, or weeping sore
People with severe eczema may need more intensive treatment to relieve their symptoms. Continuous rubbing and scratching can also lead to skin infections. Refer to dermatology if AD is:
- With severe skin bacterial infection that requires oral/ IV antibiotics
- Acute erythroderma affecting more than 80% of body surface area
- Severe and uncontrolled eczema with frequent infections
- Diagnostic uncertainty
What is Sensitive Skin?
Sensitive skin is a syndrome defined by unpleasant sensations in response to stimuli that normally does not provoke such sensations. The face is the most common site of sensitive skin. 61% of women and 32% stated that they have experienced sensitive skin on the face. Common characteristics of sensitive skin include dry and impaired (damaged) skin.
Triggering Factors
There are many potential aggravating factors which can worsen flares in AD and sensitive skin, either independently or in combination. Potential triggering factors include the following:
- Aeroallergen
E.g. House dusts, unfamiliar pets - Physical irritants
E.g. Chemical reagents, fragrance - Food
E.g. milk, egg and peanut - Patient factors
E.g. Stress, family history - Leaky gut syndrome
A condition in which the tight junctions of intestinal lining break apart, causing harmful substances to enter bloodstream, leading to inflammation - Weakened immune system
When triggered by a substance inside or outside the body, the immune system responds by producing inflammation.
Treatments
For patients with mild AD symptoms, topical medications are the primary choice of treatment. However, if the basic and topical therapies fail, a systemic approach may be necessary.
- Topical corticosteroid cream (TCS)
Short term use of topical corticosteroid cream acts as first line treatment during acute flare. TCS cream works as anti- anti-inflammatory agent and has an immuno-suppressant effect. It suppresses the release of mediators such as histamine and prostaglandin that cause itchiness and inflammation. Choice of potency depends on the age, severity and site of skin lesions. TCS should be used concomitantly with emollients. (Wait 10-15 minutes after applying an emollient before applying a topical steroid). After resolution of eczema flares, discontinuation of TCS application should be done gradually to avoid rebound (i.e. twice a day followed by once a day then 1 – 3 times a week before complete discontinuation). The continuous use of TCS should be limited to 2 weeks in a row. - Topical calcineurin inhibitor (TCI)
Topical calcineurin inhibitors are considered as an alternative for patients unresponsive or intolerant of other topical therapies. It inhibits inflammatory cytokine transcription in activated T-cells & other inflammatory cells through inhibition of calcineurin. The use of TCI may be considered to treat flares in patients ≥ 2 years old and is suitable on all body locations (especially the face, hands and feet). Patients are advised to avoid excessive exposure to UV light and continue the treatment for another 1 week after signs and symptoms of atopic dermatitis have cleared. Examples of TCIs are Pimecrolimus and Tacrolimus. European Guidelines indicate that pimecrolimus is the preferred choice for sensitive skin areas and has a good safety profile for long term use. - Anti-infectious agents (Topical or Oral)
Infections of bacteria, viruses, and fungi can frequently accompany AD, and symptoms of AD can be aggravated following an infection. Any secondary infection should be controlled. Topical or oral antibiotics will be prescribed if eczema occurs alongside with bacteria infection. - Oral antihistamine
Antihistamines relieve histamine-induced itching sensations by blocking H1 receptors. Sedative antihistamine helps prevent scratching during sleep and may offer symptomatic relief for itching that worsens at night. - Systemic therapy
Systemic therapies using pharmaceutical drugs, such as glucocorticoids, cyclosporin, methotrexate, mycophenolate, azathioprine, are generally reserved for patients with severe and refractory AE. These agents must be used carefully, with consideration of their potential adverse effects.
Self-Care Tips In Treating AD
- Wet wrap therapy
It consists of 2 layers of bandage/ garments with inner wet and outer dry layer; applied over emollient alone or with combination of TCS (7-14 days). This method helps to rehydrate and calm the skin, enabling topical medications to work better. - Good bathing practice
Avoid the use of extreme temperatures (too hot or too cold) during bathing. Pat dry skin after shower, do not rub (as this can cause skin thickening, darkening and may lead to further complication including bacterial infection). Use a mild soap, skin cleanser with low PH. - Daily skincare
Applying moisturizer daily helps prevent excessive drying of the skin throughout the day. Creams, ointments and lotions seal in moisture. Choose a product or products that work well for you or ask the caring pharmacist for more information.
- Identify and avoid the aggravating factors
Make an allergy diary to help identify allergens and avoid them. Learn how to manage stress as it could be one of the triggering factors for AD.
Summary
Most AD patients have a chronic, relapsing disease course characterized by remission and intermittent flares. Although there is currently no cure for eczema, the flare can be treated and prevented with proper skincare routine, medication and lifestyle changes. To find out more information regarding skin care tips, you may consult the pharmacist in your nearby CARiNG Pharmacy.
References:
- Nutten S: Atopic Dermatitis: Global Epidemiology and Risk Factors. Ann Nutr Metab 2015;66(suppl 1):8-16. doi: 10.1159/000370220
- Clinical Practice Guideline Atopic Dermatitis 2018
- van Zuuren EJ, Fedorowicz Z, Christensen R et al. Emollients and moisturisers for eczema. Cochrane Database Syst Rev. 2017; 2:CD012119
- Enomoto, T., Sowa, M., Nishimori, K., Shimazu, S., Yoshida, A., Yamada, K., et al. (2014). Effects of bifidobacterial supplementation to pregnant women and infants in the prevention of allergy development in infants and on fecal microbiota. Allergol. Int. 63, 575–585. doi: 10.2332/allergolint.13-OA-0683
- Wollenberg A, Barbator S, J Ring, et al. Consensus-based European guidelines for treatment of atopic eczema (atopic dermatitis) in adults and children: part I (2018) Eur Acad Dermatol Venereol
Brought to you together with:

Latest Health Info
Brave the Cold: Winter Travel Needs
Winter travel has its kind of magic — snow-covered landscapes, cozy lodges, hot drinks, and festive markets. But traveling in ...
Beat the Heat When Travelling
Whether you’re on a scenic beach vacation or exploring a busy city, hot weather can quickly wear you out and ...
Got Pins & Needles? Learning about Diabetic Neuropathy
Diabetic neuropathy is a common yet serious complication of diabetes, estimated to affect up to 50% of people with the ...



